Lost Your Job? These Are Your Health Insurance Options
By The Bailey Group Marketing
Published March 31, 2017

Losing a job is one of the worst feelings on the planet, especially if it’s a job you actually enjoyed.
In addition to the feelings of anger, depression, fear, and grief, you’re now saddled with the responsibility of finding new health insurance if your company was the one providing your coverage.
Luckily, you have a number of options available to you after losing job-based coverage that you should begin to explore as quickly as possible, starting with …
Primary Options For Coverage After a Job Loss
Coverage from Your Spouse or Domestic Partner’s Employer
If your spouse or domestic partner’s insurance plan is open to family members, you may be able to join now that you no longer have insurance through your employer.
Under the Health Insurance Portability and Accountability Act (HIPAA), you have 30 days from the time that your former employer stops paying for your insurance to enroll in your spouse or domestic partner’s plan. This rule stands even if your loss of coverage doesn’t occur during an open enrollment period.
Coverage from the Marketplace
These are the types of questions you’ll need to answer in order to qualify for a Special Enrollment Period.
Under the Affordable Care Act (ACA), you can enroll in a health plan in the Marketplace during a Special Enrollment Period if you lose your job-based coverage outside of the normal open enrollment period. You may even be eligible for subsidies for reduced premiums and you might qualify for lower out-of-pocket costs.
Keep in mind that you only have 60 days from the event happening to enroll in a new plan through the marketplace.
If you’re in Florida and in the market for a Florida Blue plan, we can help you narrow down your choices and get you enrolled – at no additional cost. Simply click here to get the process started.
Coverage from the Individual Market
If you don’t qualify for a subsidy for reduced premiums from the Marketplace, you can simply sign up for a new plan off of the marketplace through the individual market. Not sure whether or not you’ll qualify for a subsidy? This interactive tool on the Marketplace’s website can help you determine that.
To sign up for an off-marketplace plan, you can either go directly to a health insurance carrier or talk to a local agent (like us!). Oh, and the same 60 day enrollment period typically applies here.
Continuing Current Coverage Through COBRA
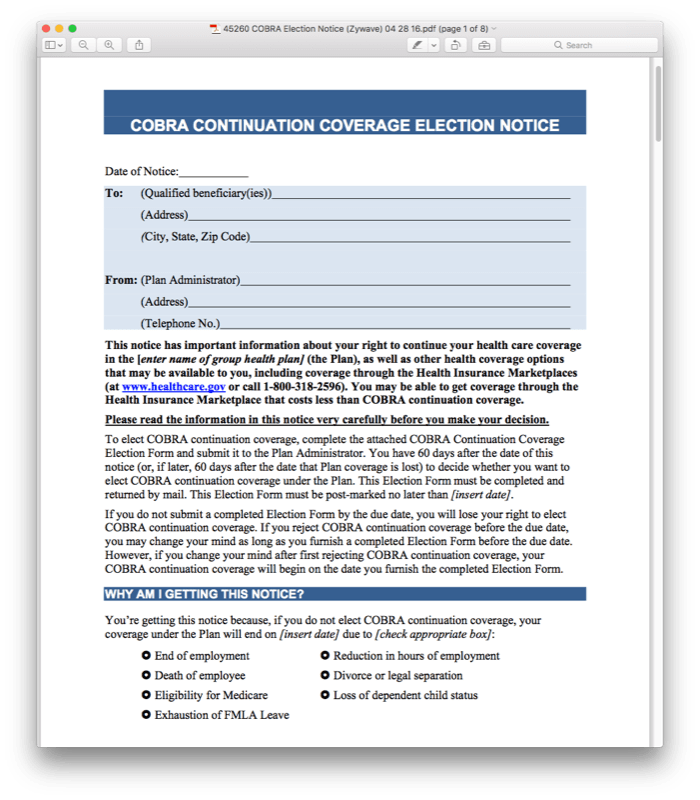
What a COBRA notice might look like from your employer.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives you the right to remain on the health plan that you had with your former employer. (COBRA does not apply if your employer had fewer than 20 employees, if your employer went out of business or if you were fired for “gross misconduct.”)
If you are eligible for COBRA benefits, you will receive notice from your former employer or the health plan, and can enroll within 60 days after receiving the notice.
- COBRA generally guarantees coverage for 18 months but may be longer depending on your circumstances.
- Each family member can make a different COBRA election, even if your entire family was once covered under your employer’s health plan. Or, your child(ren) may elect COBRA on your plan and you may find coverage elsewhere.
- You are responsible for paying the full COBRA premiums, which includes the amount you used to pay while employed, the amount paid by your former employer and an administrative fee. This can make COBRA coverage very expensive.
We recommend exploring the first 3 options above before looking into COBRA coverage as COBRA is likely to be your most expensive option for continuing coverage.
Secondary Options for Coverage After a Job Loss
State-Sponsored Programs
There may be state laws that compliment federal COBRA regulations or other consumer protection statutes. They include:
- Mini-COBRA plans. If you worked for an employer with 20 or fewer employees, your state may have mini-COBRA laws that allow you to obtain the same benefits by paying the full premium (or more in some states).
- Conversion policies. If you cannot continue coverage with your former policy, your state may require insurers to convert your policy into an individual plan.
Protections Under HIPAA
Under this federal law, at least one insurer must sell you a health plan if you can meet the following conditions:
- You previously had 18 months of coverage without a break for more than 63 days.
- The last day of your coverage was through your employment.
- You do not have a COBRA or mini-COBRA option available.
Trade Adjustment Assistance (TAA) Reauthorization Act and Health Coverage Tax Credit
If you lost your job due to a trade policy (moving your job overseas), you may qualify for 72.5 percent of the cost of your health insurance for up to three years under TAA. To learn more about this, visit the IRS’ website.
Medicaid, The Children’s Health Insurance Program (CHIP) or VA Coverage
Medicaid is available for low-income individuals and children, parents with dependent children, permanently disabled individuals or those over 65. Eligibility varies from state to state.
- Though you may not qualify for full Medicaid benefits, you may be eligible for screenings for breast and cervical cancer or assistance with tuberculosis or sickle cell anemia treatments.
- Consult your local health department for more information about public coverage options in your area.
Helpful Resources: